800-487-3808
800-487-3808

Our shoulder complex is made of three major bones: the humerus (upper arm), scapula (shoulder blade), and clavicle (collar bone). In order to maintain healthy shoulder function, all these bones need to work together fluidly and incoordination. A major injury to any of these bones, or to the muscles surrounding them, can result in fault biomechanics and even instability in the shoulder.
The major threat of shoulder joint instability is a dislocation. This occurs when the ball on the top of your humerus is forced out of its socket, most often because of sudden high impact injury. Additionally, instability can result from gradual wear and tear within the shoulder joint that causes issues like subluxation with use. Instability of the shoulder can be short- or long-term, but chronic shoulder instability typically begins with a single significant dislocation and can lead to chronic impairments.
Depending on the specific bones or muscles that are damaged, symptoms can appear in different locations around the shoulder. The shoulder joint itself is the most common type with local symptoms. Yet, in the case of shoulder blade instability, pain and other symptoms will be more prominent around the scapula and parts of the upper back.
Symptoms vary significantly depending on the type of shoulder instability you are dealing with. Whether left or right shoulder instability is present, the specific type of injury is determined by the individual parts of the joint that are damaged, discoordinated, or weakened.
It’s also important to note that instability and dislocation can each cause the other (it’s definitely not always back and white). For example, if local tissues are hypermobile from a previous injury or genetics, this can put an individual at a higher risk for dislocation. Whereas, a sudden injury that causes a dislocation will result in shoulder instability due to resulting tissue damage.
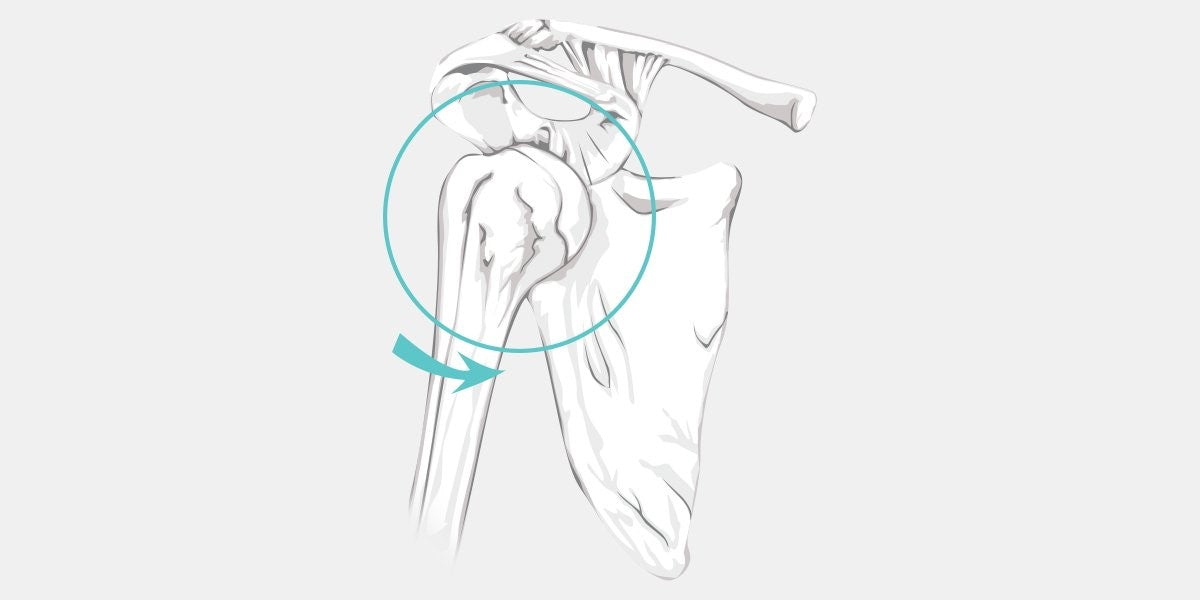 Anterior instability is the most common type of shoulder instability.
Anterior instability is the most common type of shoulder instability.
In fact, experiencing instability of the front of the shoulder joint accounts for more than 95% of dislocations. It is defined as a shift of the arm bone (specifically the ball of the joint called the humeral head) toward the front of the body. Anterior shoulder instability can be caused by an unexpected fall, especially if the victim tries to brace themselves with an outstretched arm. It is also common among athletes that are reaching overhead, such as volleyball speakers and baseball pitchers.
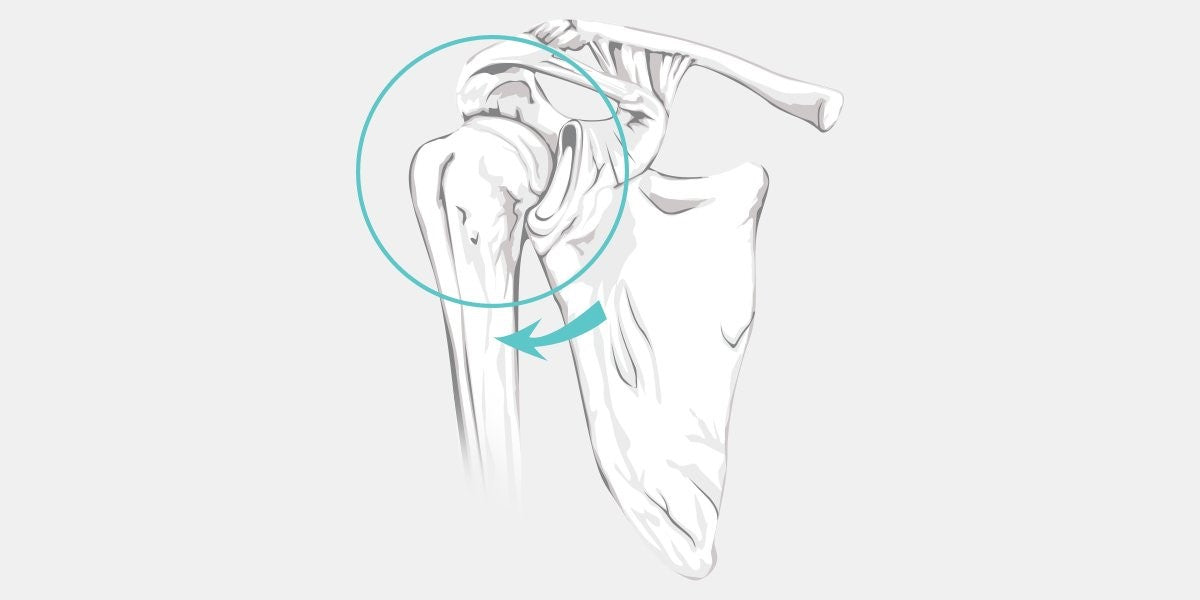 Those who suffer from seizures are most at risk of developing posterior shoulder instability.
Those who suffer from seizures are most at risk of developing posterior shoulder instability.
The mirror image of anterior instability, the posterior version of the condition is much rarer. It is most often caused by seizures or electric shocks, which can dislocate the shoulder and move it backward past its socket (also known as the glenoid).
Also called atraumatic shoulder instability, multidirectional instability of the shoulder is not caused by a sudden dislocation but a general weakness of the joint from faulty mechanics, overuse, and/or genetics. The laxity of the muscles and tendons in the region can cause the humerus to pop out of place unexpectedly. Multidirectional shoulder instability is a long-term condition that is sometimes treated with surgery.
Shoulder instability causes fall into two broad categories: traumatic and atraumatic. Traumatic instability comes from a sudden injury, often a sporting accident or fall. Atraumatic instability is a long-term condition that results from the gradual wearing down of the bone and tendons.
However, some people simply have looser shoulder ligaments from birth. In these cases, right and left shoulder instability is roughly symmetrical, affecting both arms equally.
While traumatic and atraumatic instability are considered two separate conditions, they are closely linked. A study by the British Journal of Sports Medicine found that the likelihood of long-term shoulder instability was increased by 26% after just one traumatic incident. Plus, the risk for experiencing another dislocation is also significantly higher.
Another important risk factor associated with shoulder instability. As we grow older, our muscles tend to weaken while connective tissue loses it’s normal flexibility and health, making joint dislocations more common. Combat this by implementing a strength training regimen and taking good care of your general health.
As mentioned above, some people are more prone to laxity in their joints than others (known as hypermobility). Specifically, conditions like Ehlers Danlos result in shoulder instability and increase the risk of dislocation.
It is possible for the symptoms of shoulder instability to fly under the radar in less severe cases until an accident or overexertion causes the joint to dislocate. However, more serious cases can be all too obvious for those experiencing it. Common symptoms include:
Shoulder instability pain will be most prominent during dislocations. Additionally, pain with arm range of motion and muscle use (which movements will vary with the type of instability).
The head of the humerus is much more prone to popping out of place.
Local muscle strength is impaired, and the shoulder may give out when under stress or rapidly fatigue, making it more prone to injury.
Faulty movements due to muscle weakness and poor alignment make it hard to efficiently move the arm without rapid fatigue and/or onset of pain.
The humerus may wobble in the joint and may not feel secure when moved. Subluxations, or a partial dislocation, are common with this sensation of joint hypermobility.
If you’ve acutely sustained a dislocation, the cause will be quite obvious. Otherwise, you and your doctor will discuss your medical history, looking for any previous injury or excessive use. A physical examination will help your doctor identify shoulder instability by assessing joint and ligament laxity, strength, and shoulder complex biomechanics.
Imaging tests, such as shoulder instability magnetic resonance imaging (MRI), can provide detailed pictures of the soft tissues surrounding the joint to see what tissues are affected, such as the joint capsule, labrum, ligaments, and rotator cuff muscles/tendons. Additionally, an X-ray can show injuries to the bone to rule out issues like fractures or bone spurs.
Determining the proper treatment options for shoulder instability requires an accurate diagnosis. Firstly, if there is a dislocation, then moving the joint back into place and stabilizing it with a splint or wrap is a great first response. From there, regardless of the cause, following up with exercise and a quality brace will ensure a fast and predictable recovery.
Chronic shoulder instability treatment may require surgical methods. Below are common and effective methods for treating shoulder instability.
Whether you are going with at-home treatment or opting for a more serious surgical procedure, rehabilitation for shoulder instability will always include an array of exercises, which can be self-directed or incorporated into a shoulder instability physical therapy program.
Choosing the right exercises for a shoulder instability exercise program is all about locating the source of your instability, whether it is anterior, posterior, or multidirectional. Before beginning any workout routine, make sure to get an accurate diagnosis from your doctor.
Find Exercises for Shoulder Instability
Splints, braces, and other types of support for shoulder instability come in all shapes, sizes, and price points. Make sure to have a full understanding of all the available options before you make your choice.
Simple and straightforward, arm slings are a good temporary solution that will allow a dislocated shoulder to heal properly by restricting movement and offering basic support. If your injury is only slight, and you don’t mind the temporary loss of functionality, a sling is a great option. Often, your doctor will prescribe the use of a sling for a specific amount of time to allow healing.
From the most basic anti-bacterial tape to full-fledged compression sleeves, wraps go the extra mile by compressing the injured muscles while also offering light support. Some compression wraps have heating or cooling features, which might speed the recovery process and keep you comfortable. Wraps are slim and lightweight, making them ideal for those who want to get back to their favorite sport.
A good shoulder brace includes a few basic features: breathable fabric, a snug fit, and maximized stability. Look for one that adjusts easily and meets the needs of your injury. A brace might allow you to resume your daily life with less pain and will help protect your injured shoulder from further damage.
Find the Best Shoulder Brace for You
Shoulder immobilizers are commonly considered post-surgery and during more severe recovery processes. While you won’t be swinging a tennis racket any time soon, they ensure a safe recovery by protecting severely injured tissues, such as a labral or rotator cuff tear.
Surgical treatment comes in many different forms and is most often used to treat long-term cases or severe acute injuries that resulted in significant tissue tears. The goal of surgery for shoulder instability is to reduce the risk of future dislocations by repairing tendons and ligaments or adding stabilizing elements to the joint.
A capsular shift is a form of multidirectional shoulder instability surgery that focuses on tightening the ligaments in the area to provide greater support. Performed with an arthroscope (shoulder arthroscopy), it is minimally invasive and affords a shorter recovery time.
Multidirectional instability shoulder surgery can also include a latarjet procedure, which involves a bone graft. This form of surgery is used in cases in which the bone has worn away significantly or is severely injured.
The shoulder instability rehab process can extend from several weeks to months after a dislocation, depending on medical history and the type of treatment. Those with first-time dislocations may resume normal activity in as soon as two weeks but typically should avoid lifting heavy objects before six weeks. However, this will vary a lot with each individual.
Exercises and braces help a dislocated shoulder regain function, which is an excellent long-term solution for many people. However, if chronic dislocations are occurring then surgery is most likely needed to make a full recovery.
Shoulder instability surgery recovery time may be much longer than that of a dislocation (but not always). Do not expect to recover fully until sixteen weeks after the initial injury, although your doctor will provide a more accurate estimate for your individual case.
Whether you are dealing with a first-time dislocation or recurring instability, taking the right steps now is the only path to long-term health. Implementing a comprehensive workout routine, using a quality shoulder brace when needed, and speaking with your orthopedic doctor about surgical options will make a major difference to your shoulder health in years to come.
Sources:
https://orthoinfo.aaos.org/en/diseases--conditions/chronic-shoulder-instability
https://www.physio-pedia.com/Anterior_Shoulder_Instability
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811734/
https://bjsm.bmj.com/content/49/14/913
Shop Shoulder Pains
Leave a comment